The current treatments for many autoimmune diseases include the systemic use of anti-inflammatory drugs and potent immunosuppressive and immunomodulatory agents (i.e., steroids and inhibitor proteins that block the action of inflammatory cytokines). In recent years, researchers have contemplated the use of stem cells to treat autoimmune disorders such as Lupus, Rheumatoid arthritis and Type 1 diabetes.
Gene therapy is the genetic modification of cells to produce a therapeutic effect. In most investigational protocols, DNA containing the therapeutic gene is transferred into cultured cells, and these cells are subsequently administered to the animal or patient. DNA can also be injected directly, entering cells at the site of the injection or in the circulation. Under ideal conditions, cells take up the DNA and produce the therapeutic protein encoded by the gene. There are several approaches for isolating and cultivating stem cells or islet precursor cells from fetal and adult pancreatic tissue. In addition, new promising studies indicate that insulin-producing cells can be cultivated from embryonic stem cell lines.
Development of Cell-Based Therapies for Diabetes
Mouse embryonic stem cells can be derived from the inner cell mass of the early embryo (blastocyst) and cultured under specific conditions. The embryonic stem cells can then be expanded and differentiated. Islet cells can be selected for further differentiation and characterisation. These cells can then be grown in culture where they spontaneously form three-dimensional clusters similar in structure to normal pancreatic islets. The cells also produce and secrete insulin. The pancreatic islet-like cells show an increase in release of insulin as the glucose concentration of the culture media is increased. The pancreatic islet-like cells became vascularized, synthesized insulin and maintained physical characteristic when implanted in the shoulder of diabetic mice.

Stem Cells Bring New Strategies for Developing Replacement Neurons
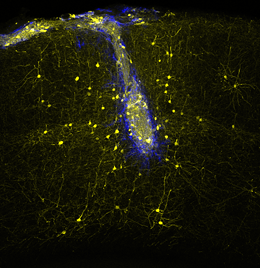
Furthermore, this same method of using mouse embryonic stem cells from the inner cell mass of the blastocyst and culturing these cells until the create embryoid bodies. The embryoid cells are differentiated. Nestin-positive neuronal precursor cells or Islet cells can be selected for further differentiation and characterisation. These cells can produce dopamine or serotonin and can be used as neurotransmitters that cross synapses and bind receptors on the neuronal cell body and dendrites. This can be a potential therapeutic treatment for Parkinson’s disease were the nigro-striatal pathway degenerates for unknown reasons.
Stem Cells’ Future Role in Spinal Cord Injury Repair
Researchers used a rat model of amyotrophic lateral sclerosis (ALS) which is a disease that destroys special nerves found in the spinal cord, known as motor neurons, that control movement. Using stem cells from fetal tissue which were cultivated under certain conditions to produce embryoid bodies that look and function like neurons. Only elected cells that displayed molecule markers of neural stem cells, including the proteins nestin and neuron specific enolase were selected for further differentiation. The prepared cells from embryoid bodies were injected into fluid surrounding the spinal cord of the paralysed rats that had damaged motor neurons. The results showed that the rats had regained motor abilities. This shows potential therapeutic treatment for patients of Motor Neuron diseases, Multiple Sclerosis, Alzheimer’s disease and Huntington disease where the nerves are damaged.